Pulmonary embolism (PE) is the third most common cause of cardiovascular death. Hospitals worldwide initiated the movement to assemble multidisciplinary teams or Pulmonary Embolism Response Teams (PERTs) to help manage PE, improve care coordination, and determine suitable treatment interventions for acute PE patients. First established in 2012 at Massachusetts General Hospital, over 100 institutions now have active PERTs.
Dr. Derlis Fleitas Sosa and co-authors performed a systemic review and meta-analysis to understand the impact of PERTs on PE management and patient outcomes.
Summary:
- A trend toward lower mortality was noted in the PERT group, despite comprising more acute PE patients.
- The PERT group had a significant increase in the use of advanced therapies and a decrease in IVC filter use.
- Bleeding rates were similar in both PERT and control groups.
Sixteen studies comprising 3827 patients in the PERT group (PERT era) and 3967 patients in the control group (pre-PERT era or a comparison group) were included in the meta-analysis. The PERT group had more intermediate- and high-risk PE patients than the control group.
A multidisciplinary team approach for PE management
PERTs immediately and simultaneously help bring together multiple specialists to coordinate care for acute PE patients. Pulmonary and critical care medicine was present in all PERTs reviewed in this study. Other specialties included interventional radiology (92%), cardiac surgery (92%), cardiology (85%) and haematology (23%).
PERT and patient mortality
A trend toward lower mortality was noted among PERT patients, even though this group had a higher number of intermediate- and high-risk PE patients. Two studies (Chaudhury P et al. and Myc LA et al.) reported a lower readmission rate in the PERT group. Chaudhary et al. noted that the mortality benefit was significant in intermediate- and high-risk PE. The authors suggest further studies on how PERTs affect mortality in intermediate- and high-risk PE patients.
PERT and advanced interventions
There was a significant increase in the use of advanced interventions (catheter-directed thrombolysis and catheter-assisted embolectomy) in the PERT group. It could be due to the higher number of intermediate- and high-risk PE patients in this group. The authors also noted the rise of more advanced interventions and risk stratification tools that coincided with the formation of PERT as a contributing factor.
Despite an increase in the use of advanced interventions to treat acute PE, there was a significant decrease in the use of IVC filter placement in the PERT group. The authors suggest PERT members were more likely to be aware of IVC-filter-related complications.
PERT and bleeding complications
PE treatment may lead to complications such as excessive bleeding, recurring blood clots, or pulmonary hypertension. Yet, the meta-analysis shows that the bleeding rates were similar in both groups, despite the use of advanced interventions in the PERT group. The authors recommend future reports of PERT outcomes should report bleeding complications in detail.
Future directions for research
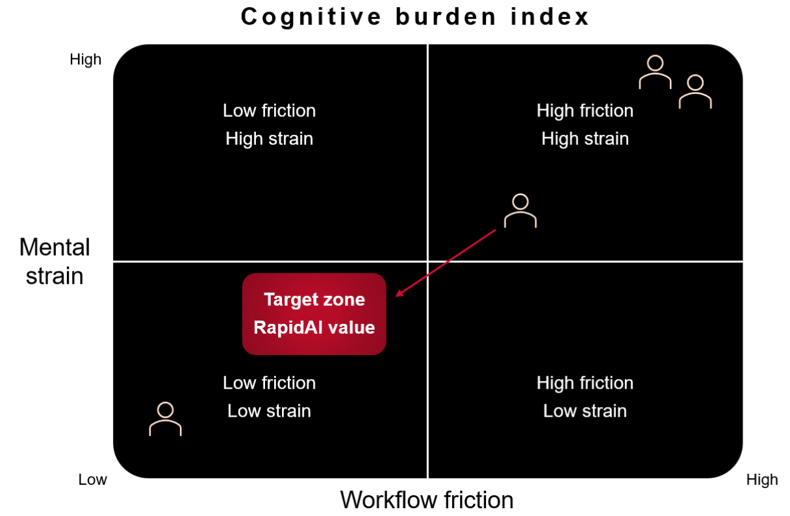
Future randomized controlled trials on PERT outcomes can help us understand the impact of these multidisciplinary teams on the outcomes of patients with acute PE. With hospitals creating VTE coordinator roles and AI tools to help accelerate decision-making and streamline PE workflow, PERTs can further improve processes and outcomes in acute PE patients in the coming years.